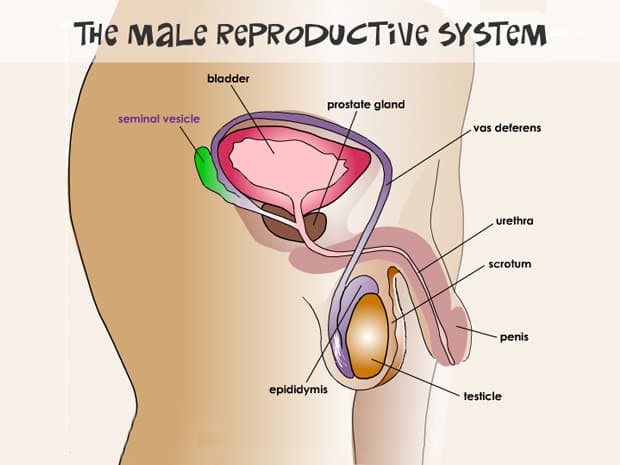
The male reproductive system is mainly outside of the body. The scrotum, penis, and testicles are among these external organs. The prostate, vas deferens, and urethra are internal organs. The male reproductive system is in charge of both urinary and sexual functions.
What is The Male Reproductive System?
A man’s reproductive and urinary systems are made up of organs known as the male reproductive system. These organs are responsible for the following functions in your body:
- Produce, transport, and maintain semen (the protective fluid around sperm) and sperm (the male reproductive cells).
- Deliver sperm into the reproductive system of females.
- Secrete and produce male sex hormones.
Internal (inside your body) and external (outside your body) elements make up the male reproductive system. These organs work together to help you urinate (get rid of liquid waste), have sexual intercourse, and make babies.
How Does The Male Reproductive System Function?
Hormones control the entire male reproductive system. These are chemicals that regulate or stimulate the activity of your organs or cells. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), and testosterone are the main hormones involved in the functioning of the male reproductive system.
The pituitary gland produces FSH and LH. It’s located at the base of your brain and is in control of a variety of body activities. FSH is essential for sperm production (spermatogenesis). LH increases the creation of testosterone, which is required for spermatogenesis to continue. Testosterone has a role in developing male characteristics such as muscle growth and strength, fat distribution, bone mass, and sexual drive.
What are The External Male Reproductive Structures?
The male reproductive system is mainly found outside of the abdominal cavity and pelvis. The penis, scrotum, and testicles are all exterior elements of a man’s reproductive system.
1. Penis
The penis is a male organ that is used for sexual behavior. It is divided into three sections:
- The Root
This is the part of the penis that connects to the wall of the abdomen.
- The Body or Shaft
The penis body is shaped like a tube or cylinder and is made up of three interior chambers. A sponge-like erectile tissue with hundreds of big holes fills these chambers with blood when sexually aroused. The penis gets hard and erect as it fills with blood, allowing penetration during sex. During an erection, the skin of the penis is loose and elastic, allowing for variations in penis size.
- The Glans
This is the penis’s cone-shaped end. The glans, often known as the head of the penis, are covered by a loose layer of skin called the foreskin. Circumcision is a procedure that removes a portion of this skin.
The urethra, the tube that takes both sperm and urine out of the body, opens at the glans penis’ tip. Many sensitive nerve endings can also be found in the penis.
When a man reaches sexual climax, semen containing sperm is discharged (ejaculated) through the end of the penis (orgasm). When the penis is erect, the urethra is blocked, enabling only semen to be ejaculated during orgasm.
2. Scrotum
The loose pouch-like sac of skin that hangs behind the penis is known as the scrotum. It contains the testicles (usually called testes) and a variety of blood arteries and nerves. The scrotum protects your testes while also acting as a climate control system.
For healthy sperm growth, the testes must be kept at a temperature slightly below body temperature. The scrotum’s wall has special muscles that may contract (tighten) and relax, allowing the testicles to slide closer to the body for warmth and protection or farther away for colder temperatures.
3. Testicles (Testes)
The testes are oval organs that lie in the scrotum and are connected by the spermatic cord at both ends. The majority of males have two testes. The testes are important for creating sperm and manufacturing testosterone, the primary male sex hormone. Through a process known as spermatogenesis, these tubules are responsible for developing sperm cells. Inside the testes are seminiferous tubules, which are coiled masses of tubes.
4. Epididymis
Each testicle has an epididymis, a long, coiled tube that sits on the backside of each testicle. It transports and stores sperm cells produced by the testes. The epididymis is also responsible for maturing sperm, as the sperm that exit from the testes are immature and unable to fertilize. Contractions in the vas deferens force sperm into the vas deferens during sexual arousal.
What are The Internal Male Reproductive Organs?
Several internal organs, often known as accessory organs, play an important role in the male reproductive system. The following organs are among them:
1. Vas Deferens
The vas deferens is a long, muscular tube that extends from the epididymis to the pelvic cavity slightly beyond the bladder. To prepare ejaculate, the vas deferens transports mature sperm to the urethra.
2. Ejaculatory Ducts
The vas deferens and the seminal vesicles merge to generate these ducts. The urethra is where the ejaculatory duct exits.
3. Urethra
The tube that conveys urine from the bladder is known as the urethra. When you experience orgasm, it also has the function of expelling (ejaculating) semen. The urine flow from the urethra is restricted while the penis is erect during sex, allowing only semen to be ejaculated at orgasm.
4. Seminal Vesicles
Seminal vesicles are sac-like pouches located near the bladder’s base and attached to the vas deferens. The seminal vesicles produce a sugary fluid (fructose) that provides energy to sperm and helps their movement (motility). The majority of your ejaculatory fluid, or ejaculate, is made up of the fluid from your seminal vesicles.
5. Prostate Gland
The prostate gland is a walnut-sized organ placed in front of the rectum, below the urine bladder. The prostate gland gives additional fluid to the ejaculate. Prostate fluids also help with sperm nutrition. The urethra goes through the middle of the prostate gland, carrying the ejaculate to be released at orgasm.
6. Bulbourethral Glands
The bulbourethral glands, also known as Cowper’s glands, are small glands found on the sides of the urethra, right below the prostate gland. These glands produce a clear, slippery liquid that drains into the urethra. This fluid lubricates the urethra and neutralizes any acidity in the urethra caused by remaining urine drops.
Clinical Significance
Low libido, failure to ejaculate, decreased bone density, muscle loss, infertility, loss of body hair, and, most critically, incomplete sexual development are symptoms of male reproductive system disorders. Low energy/depressed mood, anemia, or increased body fat are less specific symptoms of low testosterone. Metabolic syndrome, insulin resistance, and atherosclerosis are some of the other comorbidities linked to low testosterone.
Can a Man Go Through Menopause?
The term “menopause” refers to the end of a woman’s normal menstrual cycle. Hormone production changes in women are a sign of this. One of the most significant changes for a woman after Menopause is the inability to produce children. Unlike the ovaries, the testes do not lose their ability to produce hormones. If a man is in good health, he may produce sperm until his 80s or beyond.
Subtle changes in the function of the testes, on the other hand, can occur as early as 45 to 50 years old and more significantly around the age of 70. Hormone production in many men may remain normal far into old life, whereas in others, it may begin to decline earlier. This can occur as a result of a medical condition such as diabetes.
It’s uncertain whether testicular failure causes symptoms such as fatigue, weakness, sadness, or impotence.
Can “Male Menopause” be treated?
Hormone replacement therapy may help ease symptoms such as a loss of interest in sex, sadness, and weariness if your testosterone levels are low. However, replacing male hormones can increase prostate cancer and atherosclerosis (artery hardening). Before beginning hormone replacement treatment, you should have a comprehensive medical examination and laboratory testing performed.
Many questions concerning how many middle-aged men could benefit from hormone replacement therapy remain unsolved. Discuss all of the benefits and drawbacks of this treatment with your healthcare physician to choose the best course of action for you.




