Reproduction is the process by which organisms make more organisms like themselves.
Two types of sex cells or gametes are involved in the human reproductive process. In the reproductive system of females, the male gamete (sperm) and the female gamete (egg or ovum) meet. When the sperm fertilizes an egg, it produces a zygote (fertilized egg). The zygote undergoes a process of embryo development and fetal development.
The male reproductive system and the female reproductive system both are essential for reproduction. However, the reproductive role of the female reproductive system is far more complex than that of a male. She not only has to produce gametes, but her body must be prepared to nurture a developing for approximately nine months.
What Parts make up the Female Reproductive System?
The female reproductive anatomy includes external and internal parts.
External Female Reproductive system
The main external structures of the female reproductive system include:
- Vulva
The exterior part of the female reproductive system is termed the vulva. The vulva between the legs covers the opening to the vagina and other reproductive organs in the body.
- Labia
Mons pubis is considered the fleshy region right above the top of the entrance of the vagina. The vaginal opening is surrounded by two sets of skin flaps called the labia.
- Clitoris
The labia meet at the clitoris, a small sensory organ located toward the front of the vulva. A skin fold termed the prepuce covers the clitoris, similar to the foreskin at the end of the penis.
The clitoris is highly responsive to stimulation, comparable to the penis, and can become erect.
- Bartholin’s glands
These drugs are situated next to the entrance of the vagina and create a fluid discharge.
Internal Female Reproductive system
The main internal structures of the female reproductive system include:
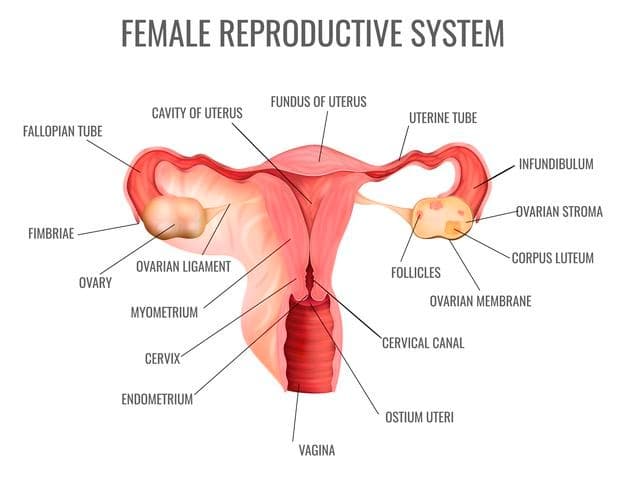
Gonads (Ovaries)
Ovaries are female gonads located in the peritoneal cavity that produce ova and release hormones. The solid, ovoid structures ovaries, about 3-5 cm long and 2-3 cm wide, flunk the uterus on each side.
There are numerous little bag formations in the ovary, each consisting of an immature oocyte termed an ovary follicle. One of the mature follicles ejects oocytes every month in adult women. The event is known as ovulation. Follicle burst after ovulation is converted into a corpus luteum glandular tissue.
Oviduct (Fallopian tube or uterine duct)
The oviducts form the initial part of the female duct system. It is the site where the ovulated egg is received for fertilization. Each oviduct has a length of around 10cm and transfers the developing ovum toward the uterus. The oocyte is transported to the uterus.
Uterus
The uterus or womb is a hollow, pear-shaped organ that is the home to a developing fetus. The uterus is divided into three portions: the fundus, the corpus, and the cervix. The oviducts join the uterus just below the fundus, and the opening of the cervix leads to the vaginal canal. The cervix, a plug of mucus in the cervix, is the lower part that opens into the vagina, and the main body of the uterus, called the corpus. The corpus can easily expand to hold a developing baby. A channel through the cervix allows sperm to enter and menstrual blood to exit.
Uterus Wall
The walls of the uterus are made up of three layers:
- The perimetrium is the outermost thin covering layer of the uterus.
- The myometrium is the middle thick muscular layer composed of smooth muscle, which contracts in rhythm during childbirth to expel the baby from the mother’s body.
- The endometrium is the spongy inner layer of the uterine cavity. The immature embryo is implanted in the endometrium after fertilization occurs and remains there for further development. A fertilized ovum must be received, retained and nurtured in the uterus.
Vagina
The vagina is a narrow 8-10 cm tube that stretches from the cervix to the body’s exterior. Often known as the birth canal, the vagina offers a channel for the delivery of an infant and menstrual flow.
Functions of the female reproductive system
The organs of the female reproductive system are responsible for:
- Production of female sex hormones
- Sexual intercourse
- Fertilization
- Production of egg (oogenesis)
- Protection and nourishment of a fertilized egg until it is fully developed
- Development of embryo
- Birth of infant
Female reproductive cycle and hormonal regulations
Cyclic events take place in the female reproductive system. The sequence of the reproductive events in the female reproductive system is known as the female reproductive cycle or menstrual cycle.
The female cycle is mainly divided into two phases, i.e. ovarian cycle and uterine cycles. The ovarian cycle events are coordinated with uterine cycle events by pituitary hormones known as gonadotropins. The cycle is split into three parts, namely menstrual, proliferative and secretory phases, based on alterations and hormonal controls.
Menstrual Phase (Days 1-5)
In this phase, the uterus releases the deeper section of its endometrium. The thick, hormone-dependent functional endometrial layer detaches from the uterus wall, a process followed by bleeding for 3-5 days. The tissue gets detached by the uterus as it flows through the vagina. The ovarian hormones are at the lowest normal levels at the start of this stage, and gonadotropins are beginning to grow. Then the levels of FSH start to grow.
Proliferative / pre-ovulatory phase (Days 6-14)
Few ovary follicles are activated by increasing the follicle-stimulating hormone (FSH) during the early days. These follicles strive for supremacy with others. As a result, all but one of those follicles cease growing and ultimately disintegrate. Still, one of the prevailing follicles in the ovary continues to become mature Graafian or vesicular follicles. Graafian or vesicular follicles cause oogenesis.
FSH also stimulates the Graafian follicle to produce estrogen, which causes the vascularization of the endometrial lining of the uterine wall. Once again, the endometrium becomes silky, thick, and well vascularized. Cervical mucus is usually thick and sticky, but increasing estrogen levels make it thin and crystalline, forming channels that facilitate sperm transmission into the cervix.
As the concentration of estrogen increases, the FSH level therefore falls. This signal for the anterior pituitary to release LH. In response to LH release, a developing egg is released from the mature follicle into the oviduct, known as ovulation. The LH also converts the ruptured follicle into a yellowish glandular mass called the corpus luteum.
Secretary/post-ovulatory phase (Days 15-28)
The endometrium prepares for the implantation of an embryo during the secretory phase. The increasing progesterone levels by corpus luteum act on the estrogen-primed endometrium, causing the arteries to elaborate and convert the functional layer into a glandular secretory layer (uterine glands). Uterine glands grow and start to separate nourishing layers of glycogen (uterine glands). The embryo is maintained until these nutrients are deposited into the rich endometrial lining of the blood.
If fertilization has not occurred, the corpus luteum will start degenerating as the LH blood level declines towards the conclusion of the secretariat phase.
Progesterone levels fall, and the endometrium cell dies, setting the stage for menstruation to begin on the 28th day.
The menstrual cycle of humans stops at the age of around 50 years and is called menopause. Cyclic menstruation is a sign of a woman’s normal reproductive life and extends between menarche and menopause.
Infertility in female
Infertility cannot be accurately described since infertility varies. A useful working definition is the failure to achieve pregnancy.
The common reasons for infertility among women are:
Failure to ovulate
Sometimes the hypothalamus or pituitary gland fails to produce hormones that result in either no follicles (lack of FSH) or egg release is affected (lack of LH).
Blocked oviduct
In some females, blockage of the fallopian tube or infections causes infertility.
Uterus damage
Fibroids are benign (non-cancerous) tumors that grow in the walls of the uterus, causing infertility.
Cervical mucus defect
During ovulation, mucus becomes thinner in the cervix, allowing sperm to swim easily. It might be difficult to conceive when there is a mucus problem.
Endometriosis
It is a disorder in which small pieces of the endometrium grow in other places, such as ovaries. This can cause infertility since it is difficult to release an egg and implant it in the womb (uterus).
Treatment of infertility
If you have infertility problems, your therapy depends on what causes the condition. Some of the treatment of infertility includes:
In Vitro Fertilization (Test Tube baby Technique)
In vitro fertilization (IVF) means fertilization outside the female body. It is the most common kind of aiding technology for reproduction. It is commonly used when the fallopian tubes are obstructed or if a male produces too little sperm. It is sometimes referred to as infant test tube technology. The method includes fertilizing one or more eggs outside the body and transmission to the uterus of fertilized eggs, known as pre-embryos.
Fertility drugs for ovulation
For women who cannot conceive because of ovulation problems, fertility medications are the most frequent therapy. These medicines control or stimulate ovulation. Consult your doctor and talk about the benefits and drawbacks of each of your alternatives for fertility medication.
Fertility restoration surgery
Uterine diseases, including endometrial polyps, uterine septic tissue, intrauterine scar tissue, and specific fibroid, can be treated with a Hysteroscopic procedure. Laparoscopy or abdominal incision cure endometriosis, pelvic adhesions, and fibroids.
Miscarriage
It’s a spontaneous birth of a fetus, generally before the 28th week of pregnancy, who is too immature to survive.
Causes
- As the fetus and the placenta grow, and the uterus stretches, the region of the placenta over the cervical opening may be torn, and bleeding may occur.
- The normally positioned placenta may tear away from the uterine wall accomplished by haemorrhaging.




